Bed sores, also known as pressure ulcers, are a significant concern in healthcare, particularly for immobile individuals. These painful wounds develop from prolonged pressure on specific body areas, damaging tissue. Understanding the susceptible body parts is crucial for effective prevention and management. In this blog, we explore the causes, risk factors, and affected areas of bed sores, offering insights to help readers recognize, prevent, and address them. From underlying mechanisms to practical strategies, this guide aims to improve awareness and outcomes in managing this often-overlooked aspect of healthcare.
Definition of Bed Sores
Bed sores, also known as pressure ulcers or decubitus ulcers, are localized injuries to the skin and underlying tissue that usually occur over bony prominences due to pressure or pressure in combination with shear or friction. These sores typically develop when an individual remains in one position for an extended period, reducing blood flow to specific body areas. Without adequate blood flow, the affected tissues become damaged, leading to the formation of ulcers.
Importance of Understanding the Affected Body Parts
For several reasons, understanding which body parts are most susceptible to bed sores is crucial. Firstly, it allows for targeted preventive measures to be implemented, such as regular repositioning or specialized support surfaces, to alleviate pressure on vulnerable areas. Secondly, knowing the commonly affected body parts helps healthcare professionals assess and monitor patients at risk for developing bed sores. Additionally, awareness of the affected body parts aids in the early detection and treatment of bed sores, thereby minimizing the risk of complications and promoting faster healing. Overall, comprehending the specific areas of the body prone to bed sores is essential for effective prevention, management, and improvement of patient outcomes.
Causes of Bed Sores
Prolonged Pressure
Prolonged pressure is the primary cause of bed sores, particularly in individuals with limited mobility or those who spend extended periods in a single position. When pressure is applied to a specific body area for an extended time, it restricts blood flow to the skin and underlying tissues, leading to tissue ischemia and, ultimately, tissue damage. Bony prominences, such as the sacrum, heels, and hips, are particularly vulnerable to pressure ulcers due to the lack of soft tissue padding to cushion against pressure.
Friction
Friction occurs when the skin rubs against a surface, such as bedding or clothing, leading to abrasions or skin tears. In individuals with compromised mobility, friction can exacerbate the development of bed sores by further damaging the skin's protective barrier and increasing susceptibility to injury. Proper positioning and appropriate bedding can help reduce friction and minimize the risk of bed sore formation.
Shear
Shear forces occur when adjacent tissue layers move in opposite directions, causing stretching and tearing of blood vessels and tissues. In bed sores, shear forces commonly happen when a person is pulled or slid across a surface, such as when repositioning in bed or transferring to a chair. These forces can disrupt blood flow and contribute to tissue damage, particularly with pressure and friction. Minimizing shear forces through careful positioning and movement techniques is essential for preventing bed sore development.
Moisture
Moisture from sweat, urine, or feces can increase the risk of bed sore formation by softening the skin and increasing susceptibility to breakdown. Prolonged exposure to moisture can lead to skin maceration, making it more prone to friction and damage. Additionally, moisture creates an ideal environment for bacterial growth, increasing the risk of infection in existing wounds. Proper skin care, including keeping the skin clean and dry, prevents moisture-related complications and reduces the risk of bed sores.
Risk Factors for Developing Bed Sores
Immobility
Immobilization significantly increases the risk of developing bed sores, whether due to illness, injury, or advanced age. Individuals who cannot change positions frequently or bear weight on different body parts are more susceptible to prolonged pressure on specific areas, leading to tissue damage and ulcer formation. Immobility also limits the ability to detect and address early signs of skin breakdown, further exacerbating the risk of bed sore development.
Poor Circulation
Poor circulation, often associated with conditions such as diabetes, peripheral vascular disease, or heart failure, impairs the delivery of oxygen and nutrients to tissues, increasing their vulnerability to pressure-related injuries. Reduced blood flow slows tissue healing and makes it more difficult for the body to respond to and repair damage caused by pressure, friction, and shear forces. Therefore, individuals with compromised circulation are at higher risk of developing severe and non-healing bed sores.
Malnutrition
Malnutrition, characterized by inadequate intake of essential nutrients, compromises the body's ability to maintain healthy skin and support tissue repair. Protein, vitamins, and minerals play crucial roles in skin integrity, collagen synthesis, and immune function, all essential for preventing and healing wounds. Malnourished individuals are more prone to developing thin, fragile skin that is susceptible to breakdown, as well as experiencing delayed wound healing and an increased risk of infection.
Age
Advanced age is a significant risk factor for bed sore development due to age-related changes in skin structure, reduced mobility, and a higher prevalence of chronic health conditions. Elderly individuals often have thinner, drier skin with decreased elasticity and collagen content, making it more susceptible to damage from pressure, friction, and shear forces. Age-related declines in sensory perception and immune function also contribute to delayed wound healing and increased susceptibility to infection, further complicating the management of bed sores in older adults.
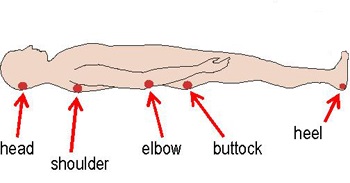
10 Commonly Affected Areas of the Body
- Sacrum
- Coccyx
- Heels
- Ankles
- Hips
- Buttocks
- Elbows
- Shoulder Blades
- Ears
- Back of the Head
Layers of Skin Affected by Bed Sores
Epidermis
The epidermis, the outermost layer of the skin, is often affected in the early stages of bed sore development. Initially, pressure ulcers may manifest as non-blanchable erythema or discoloration of the skin, indicating damage to the epidermis caused by prolonged pressure and ischemia. If timely intervention is not implemented, epidermal breakdown may progress to more severe stages, leading to the formation of open wounds and ulceration.
Dermis
As bedsores advance, they penetrate deeper into the skin layers, reaching the dermis—the layer beneath the epidermis that contains blood vessels, nerves, and connective tissue—damage to the dermis results in partial-thickness wounds characterized by shallow ulceration, blistering, or shallow craters. The dermal layer plays a crucial role in wound healing by providing blood supply and structural support to the skin. It is essential to address dermal damage promptly to prevent further deterioration.
Subcutaneous Tissue
In more severe cases, bed sores extend into the subcutaneous tissue—the layer of fat and connective tissue beneath the dermis. Subcutaneous involvement indicates full-thickness wounds that penetrate the skin layers, exposing underlying tissues to injury and infection. Damage to subcutaneous tissue can lead to the formation of deep, crater-like ulcers with visible adipose tissue or necrotic debris, requiring comprehensive wound care and surgical intervention to facilitate healing.
Muscles and Bones
In the most advanced stages of bed sore development, ulcers may penetrate the subcutaneous tissue to involve underlying muscles, tendons, and even bones. Damage to muscle tissue can result in muscle necrosis and atrophy, leading to functional impairment and prolonged recovery. Bone involvement increases the risk of osteomyelitis—an infection of the bone—which can be challenging to treat and may require surgical debridement or bone resection. Prevention of deep tissue injuries and early intervention is critical for minimizing the risk of muscle and bone involvement in bed sore patients and optimizing treatment outcomes.
Prevention and Treatment
Positioning and Repositioning
Proper positioning and regular repositioning are fundamental for preventing bed sores in individuals at risk. Encouraging changes in position every two hours helps redistribute pressure and relieve areas prone to pressure ulcers. Caregivers should use positioning aids such as pillows, foam wedges, and specialized support surfaces to maintain proper alignment and reduce pressure on vulnerable body areas.
Skin Care and Hygiene
Maintaining good skin hygiene is crucial for preventing bed sores. Regular skin inspection for signs of redness, warmth, or changes in texture helps identify early signs of skin breakdown. Cleansing the skin gently with mild soap and water and patting it dry helps remove irritants and moisture, reducing the risk of skin breakdown. Moisturizers can help keep the skin hydrated and supple, enhancing its protective barrier against friction and shear forces.
Nutrition and Hydration
Proper nutrition and hydration are essential in supporting skin health and wound healing. Adequate protein, vitamins, and minerals intake is crucial for maintaining skin integrity and helping tissue repair. Hydration is equally important for keeping the skin hydrated and facilitating nutrient delivery to tissues. Individuals at risk of bed sores should consume a balanced diet of fruits, vegetables, lean proteins, and whole grains and ensure adequate fluid intake to support skin health.
Support Surfaces and Devices
Support surfaces and devices can help reduce pressure and shear forces on vulnerable body areas, minimizing the risk of bed sore development. Specialized mattresses, overlays, and cushions designed to redistribute pressure can provide additional support and comfort for at-risk individuals. Wheelchair cushions, heel protectors, and other assistive devices can help alleviate pressure on specific body parts and prevent skin breakdown.
Wound Care and Dressings
Proper wound care is essential for treating existing bed sores and preventing complications. Wounds should be cleaned with a gentle saline solution to remove debris and bacteria, and appropriate dressings should be applied to promote healing and protect against infection. Advanced wound care products such as hydrocolloids, foams, and films may manage exudate, maintain moisture balance, and facilitate granulation tissue formation.
Surgical Interventions
In severe bed sores, surgical interventions may be necessary to remove necrotic tissue, improve wound healing, and prevent complications. Surgical debridement involves removing dead or infected tissue from the wound bed to promote healthy tissue regeneration. Flap reconstruction techniques may be used to cover large or deep wounds and restore skin integrity. Surgical interventions are typically reserved for advanced-stage bed sores that have not responded to conservative treatment measures and require more aggressive management to achieve healing.
Conclusion
A thorough understanding of the causes, risk factors, and affected body areas of bed sores is essential for effective prevention and management. Key considerations include the importance of regular repositioning, maintaining optimal skin hygiene, and addressing underlying factors such as immobility and malnutrition. Early identification and intervention are paramount in halting the progression of bed sores and reducing associated complications. Looking ahead, advancements in support surfaces, wound care technologies, and interdisciplinary care approaches hold promise for improved prevention and treatment outcomes. By proactively implementing these measures and remaining vigilant in identifying early signs of skin breakdown, healthcare professionals and caregivers can collaboratively minimize the impact of bed sores and enhance overall patient well-being.


.webp)

.avif)