We will explore the definition and significance of second-degree burns, shedding light on their distinction from first-degree burns. Understanding the nuances between these burn types is vital for accurate assessment, effective treatment, and minimizing potential complications. Join us as we explore the characteristics, causes, treatment options, and long-term care associated with second-degree burns, equipping you with valuable insights for managing these injuries with confidence and care.
Definition of Second-Degree Burn
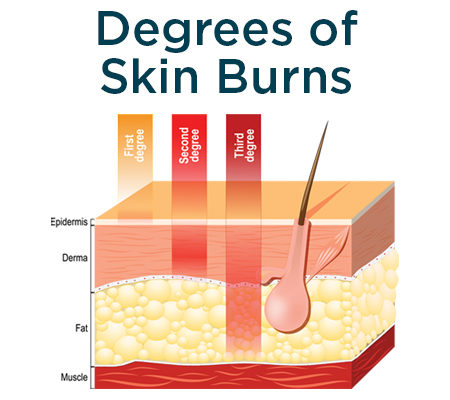
A second-degree burn, medically termed a partial-thickness burn, is a type of skin injury that affects the outermost layer, known as the epidermis, and extends into the underlying layer, the dermis. This type of burn is typically characterized by symptoms such as redness, swelling, blistering, and significant pain. Unlike first-degree burns, which only affect the epidermis and are often minor, second-degree burns involve damage to deeper layers of the skin, making them more severe and requiring a different level of care.
Second-degree burns can occur due to various heat sources, such as scalding liquids, flames, hot objects, or exposure to chemicals or electricity. The severity of a second-degree burn can vary depending on factors such as the duration and intensity of the heat exposure, the individual's age, and overall health. In some cases, second-degree burns can lead to complications such as infection, scarring, and impaired function of the affected area if not properly treated.
The Importance of Understanding Different Degrees of Burns
Understanding the various degrees of burns, including the distinction between first and second-degree burns, is crucial for proper assessment and treatment. While first-degree burns only affect the outer layer of the skin and often heal on their own with minimal intervention, second-degree burns involve more profound tissue damage. They may require medical attention to prevent complications such as infection and scarring. Recognizing the severity of a burn helps determine the appropriate course of action for optimal recovery and outcome.
Understanding Burn Degrees
Explanation of First, Second, and Third-Degree Burns
Burns are classified into different degrees based on the depth and severity of tissue damage they cause. Understanding these degrees is crucial for accurate assessment and appropriate treatment. Here's a breakdown of each degree:
First Degree Burns:
- First-degree burns, also known as superficial burns, affect only the outer layer of the skin, known as the epidermis.
- These burns are characterized by redness, pain, and minor swelling. They may also cause mild to moderate discomfort.
- First-degree burns include mild sunburns or brief contact with a hot surface.
Second Degree Burns:
- Second-degree burns, also called partial-thickness burns, extend beyond the epidermis and affect the underlying layer of skin, known as the dermis.
- These burns are characterized by symptoms such as redness, blistering, swelling, and intense pain. The skin may appear moist or weeping due to fluid buildup in the damaged tissue.
- Second-degree burns are typically caused by exposure to hot liquids, flames, chemicals, or prolonged sun exposure.
Third Degree Burns:
- Third-degree burns, also known as full-thickness burns, extend through the entire skin thickness and may damage underlying tissues such as muscles, bones, and nerves.
- These burns often result in charred or white-colored skin and may be accompanied by numbness due to nerve damage. They may appear leathery or waxy in texture.
- Third-degree burns require immediate medical attention and may necessitate skin grafting or other surgical interventions for proper wound closure and healing.
Differentiating Characteristics of Each Degree
First Degree Burns vs. Second Degree Burns:
First-degree burns only affect the epidermis, causing redness and mild pain, whereas second-degree burns extend into the dermis, leading to blistering, more intense pain, and potential scarring.
First-degree burns typically heal within a few days with minimal intervention, while second-degree burns may take longer to heal and may require medical treatment to prevent infection and promote proper healing.
Second-Degree Burns vs. Third-Degree Burns:
Second-degree burns involve damage to both the epidermis and dermis, causing blistering and intense pain. In contrast, third-degree burns extend through skin thickness and may involve deeper tissues.
Second-degree burns often result in significant pain and may heal with scarring. In contrast, third-degree burns may result in loss of sensation and require surgical intervention for wound closure and skin grafting.
Understanding the differences between these burn degrees is essential for accurate diagnosis, treatment planning, and optimal outcomes for individuals affected by burns of varying severity.
Identifying Second-Degree Burns
Signs and Symptoms
Second-degree burns present a distinct set of signs and symptoms that differentiate them from other degrees of burns. Recognizing these indicators is crucial for prompt and appropriate treatment. Here are the key signs and symptoms of second-degree burns:
Redness: Second-degree burns often manifest as reddened skin in the affected area. This redness may be widespread or localized, depending on the extent of the burn injury.
Blistering: One of the hallmark features of second-degree burns is the formation of blisters. These fluid-filled sacs develop due to damage to the deeper layers of the skin, specifically the dermis. Blisters can vary in size and may be present singly or in clusters.
Swelling: Second-degree burns commonly cause swelling in the affected area. This swelling occurs due to inflammation and fluid accumulation in the damaged tissue. It may contribute to discomfort and reduced mobility, mainly if the burn affects a joint or a large body area.
Pain: Second-degree burns are typically associated with significant pain, which can range from moderate to severe. The burn injury affects the nerve endings in the dermis, leading to heightened sensitivity and discomfort. The pain may be exacerbated by movement, pressure, or exposure to heat.
Moist or Weeping Skin: The skin affected by a second-degree burn may appear wet or weeping due to fluid release from damaged blood vessels and tissue. This moisture can contribute to a sensation of dampness and may increase the risk of infection if not properly managed.
Duration and Healing Process
Timeframe for Healing
The healing process of second-degree burns can vary depending on factors such as the size and depth of the burn, the individual's overall health, and the effectiveness of treatment. While some second-degree burns may heal relatively quickly with proper care, others may require more time and medical intervention. Here's a general overview of the healing timeline for second-degree burns:
Initial Treatment: Immediate first aid measures, such as cooling the burn with cool (not cold) water, applying a sterile dressing, and taking over-the-counter pain relievers, can help alleviate symptoms and prevent further damage. Seeking medical attention is crucial, especially for more extensive or more severe burns.
Acute Phase: During the first few days following the burn injury, the body initiates the inflammatory response to remove damaged tissue and begin healing. Redness, swelling, and pain are common during this phase. Blisters may also form as the body attempts to protect the underlying tissue.
Reepithelialization: As the inflammatory response subsides, the body regenerates new skin cells to cover the wound. This process, known as reepithelialization, typically begins within a few days to a week after the burn injury. The formation of new skin tissue gradually closes the wound and reduces the risk of infection.
Resolution of Symptoms: Over time, the redness, swelling, and pain associated with the burn diminish as the skin heals. Blisters may rupture and drain, leading to the formation of a protective scab over the wound. It is essential to avoid picking at or removing the scab, as it helps protect the underlying tissue during the final stages of healing.
Scar Formation: Depending on the severity of the burn and individual factors, second-degree burns may result in scarring. The appearance of scars can vary, ranging from mild discoloration to raised or depressed areas of skin. Scars may become less noticeable with time and appropriate scar management techniques, such as massage and silicone gel sheets.
Appearance of Second-Degree Burns
Second-degree burns exhibit distinct visual characteristics that differentiate them from other degrees of burns. Understanding these features is crucial for accurate identification and appropriate management. Here's a detailed overview of the appearance of second-degree burns:
Redness: Second-degree burns typically present with significant redness in the affected area. The redness may vary in intensity depending on the severity of the burn and the individual's skin tone. It often extends beyond the immediate injury site and may be accompanied by warmth and tenderness.
Blistering: One of the hallmark features of second-degree burns is the formation of blisters. These fluid-filled sacs develop as a protective response to burn injuries, cushioning and protecting the underlying tissue. Blisters may vary in size, ranging from small vesicles to larger bullae, and may appear transparent or cloudy.
Swelling: Second-degree burns often lead to swelling in the affected area due to inflammation and fluid accumulation. The degree of swelling may vary depending on factors such as the size and depth of the burn and the individual's overall health. Swelling may contribute to discomfort and reduced mobility, especially if the burn affects a joint or a large body area.
Moist or Weeping Skin: The skin affected by a second-degree burn may appear wet or weeping due to fluid release from damaged blood vessels and tissue. This moisture can contribute to a sensation of dampness and may increase the risk of infection if not properly managed. It is essential to keep the burn clean and dry to prevent complications.
Variable Texture: The skin's texture in the area of a second-degree burn may vary depending on the depth of the injury. Portions of the skin may appear intact with areas of intact blistering, while other areas may exhibit raw or denuded skin. The skin may feel tender; in some cases, there may be areas of exposed dermis.
Pain and Sensitivity: Second-degree burns are typically associated with significant pain and sensitivity. The burn injury affects the nerve endings in the dermis, leading to heightened sensitivity and discomfort. Pain may be exacerbated by movement, pressure, or exposure to heat.
Color Changes: As the burn begins to heal, the appearance of the affected area may change. Initially, the burn site may appear red and inflamed. Over time, the redness may fade, and the skin may develop a pink or light brown hue. Sometimes, the skin may darken or appear hyperpigmented in response to the injury.
Long-term Care and Management
After the initial treatment of second-degree burns, ongoing care, and management are essential for optimal healing and to minimize long-term complications such as scarring. Here are the critical aspects of long-term care and management:
Follow-up Care Instructions
Medical Follow-up: It is essential to follow up with a healthcare provider regularly to monitor the progress of the burn wound. Depending on the severity of the burn and individual factors, follow-up appointments may be scheduled to assess healing, address any complications, and adjust treatment as needed.
Wound Care: Proper wound care promotes healing and prevents infection. Follow any specific instructions your healthcare provider provides regarding dressing changes, wound cleaning, and application of topical medications. Keep the burn area clean and dry to reduce the risk of infection.
Pain Management: Continue to manage pain and discomfort associated with the burn as needed. Over-the-counter pain relievers or prescription medications prescribed by your healthcare provider can help alleviate pain and improve comfort during healing.
Activity Modification: Depending on the location and extent of the burn, you may need to modify your daily activities to avoid placing excessive strain or pressure on the affected area. Avoid activities that may cause friction or trauma to the healing skin, and follow any activity restrictions provided by your healthcare provider.
Conclusion
Comprehending the intricacies of second-degree burns is essential for managing them effectively and achieving the best possible results. By identifying the unique signs and symptoms, distinguishing between first and second-degree burns, and selecting appropriate treatment approaches, individuals can expedite healing and reduce the likelihood of complications. Vigilant long-term care and supervision, encompassing adherence to follow-up instructions and adopting preventive measures to mitigate scarring, are pivotal in fostering skin health and promoting recovery. Timely medical attention, conscientious wound care, and proactive management of scars empower individuals to navigate the aftermath of second-degree burns confidently, ensuring favorable outcomes and preserving skin integrity over the long term.


.webp)

.avif)